Can Surgery Guarantee Improvement for FAI?
Surgery Is Often Pitched as a Cure-All for FAI, but It’s Not Necessarily What You Need. Success Rates and Patient “Satisfaction” Can Be Less than What They Seem.
Table of Contents
- Studies Claim FAI Surgery Is Highly Effective
- “Surgery Success” Scoring: What It Really Tells Us
- A Better Measure of Success for FAI Surgery: Patient Motivations and Expectations Vs. Outcomes
- So, Does Surgery, in Fact, Resolve Hip Pain Problems?
- Do Studies Show Patients Are Satisfied with Surgery for FAI?
- Randomized Controlled Trials Show Little Benefit to Hip Surgery for Femoroacetabular Impingement
- Does Hip Surgery Protect Your Hip Joint from Further Damage?
- FAI Surgery: The Bottom Line
- Non-surgical Hope for Hip Pain Sufferers

If you're considering surgery for Femoroacetabular Impingement, or FAI, you've probably heard some very optimistic numbers related to success rates for arthroscopic hip surgery. Physicians sometimes convey the idea, intentionally or unintentionally, that the surgery is a surefire way to fix hip pain. People from around the world email me saying their surgeons are 90 percent certain surgery will solve their FAI hip pain.
And yet we hear a never-ending chorus of hip surgery patients say that their hips are no better after surgery.
So, what is the real FAI surgery success rate?
If you're seriously considering the surgery, it's helpful to take a look at medical research as far as actual outcomes for this procedure.
In this post, we'll consider several peer-reviewed studies in respected journals that claim high success rates so that we can take a deeper look at how “success” for surgery is calculated, and, in turn, uncover the true levels of patient satisfaction from FAI surgery.
At the bottom of this page, you'll find a list that we intend to keep updated on studies on FAI surgery satisfaction rates.
Watch this video for the highlights of research on success rates for hip impingement surgery.
Studies Claim FAI Surgery Is Highly Effective
In the 2009 study “Arthroscopic Femoroplasty in the Management of Cam-type Femoroacetabular Impingement,” 83 percent of patients were reported to have had improvement from surgery for cam and mixed (cam and pincer) impingement.
The study notes that the average improvement for those who experienced relief was 20 points on the Harris Hip Score. The range of scores went from -17 (meaning someone got much worse) to +60 (meaning someone felt much better).
On its face, a study like this sounds very promising, but the reality is much different if you break it down.
“Surgery Success” Scoring: What It Really Tells Us
The key here is to look closely at the Harris Hip Score questionnaire. It will show you what "improvement" really means.
The Harris Hip Score is a series of questions that get answered pre- and post-operation. In general, to be considered a successful hip surgery, the patient must score at least 20 points higher post-op than they did pre-op. The way the points are tallied is a flawed metric that does not actually line up with what a person with hip pain would consider success!
Let's look at a key question: How difficult is it to get 20 points?
The answer is NOT VERY. Let's examine why.
Open the Harris Hip Score questionnaire so you can follow along and test this out yourself. The very first question is about pain. Go ahead and fill in that you have "marked pain" (one step better than the very worst). Scroll down and look at your score. You should see 10.
(For a video walk-through of this section, please watch this YouTube video).
Now select "mild pain." This level corresponds to having no pain for average activities and rarely having moderate pain for unusual activities for which you might take aspirin. Scroll down and look at your score. Your score should now be 30. You have just earned 20 points, a stunning 300 percent increase, and yet your pain has not been resolved. Would you consider still having pain sometimes and taking painkillers for it a success?
Another scenario: If you select "none or ignores it" your score jumps to 44 points, a 34-point increase over your marked pain score of 10! Imagine if at a follow-up appointment your doctor asks you, "How is the pain?" and you say, "Well, it's still there, still annoying, but I can ignore it and move on with my life." You just earned top marks and the surgery would be a smashing success.
Now reset your questionnaire and look at the section title “Limp." Select "severe" and look at your score. You should see a 0. Then select "slight." Scroll down. You just earned 8 points.
So let's say you go from marked pain with a severe limp down to mild pain with a slight limp. Is that a success to you? It's an improvement of 28 points; the surgery is considered an absolute unquestionable success based on the Harris Hip Score.
The reality of this study is that improvement in quality of life did not need to be very pronounced for the surgery to be considered a success.
You have to ask yourself whether this level of "improvement"
- is worth your money and time
- supports or undermines the contention that surgery actually addresses the root cause of your problem.
A Better Measure of Success for FAI Surgery: Patient Motivations and Expectations Vs. Outcomes
If metrics like the Harris Hip Score don’t accurately reflect improvement, a better way to get true patient feedback might be to survey patient satisfaction.
Another study, published in 2012, “Fulfillment of patient-rated expectations predicts the outcome of surgery for femoroacetabular impingement,” looked at 86 patients' experiences with surgery to fix their FAI. Researchers considered the patients’ motivations and expectations for surgery to see how that affected outcomes.
The patients had common motivations for getting surgery. The top reason was to alleviate pain. The second and third reasons were a fear of the pain worsening and a desire to improve everyday activities, respectively.
Their expectations were also quite normal: 57 percent of patients expected their hip pain to get "much better" and 40 percent expected the pain to be "better," post-surgery. Also: 46 percent expected their ability to do sports would be "much better," and 37 percent expected it to be "better."
People want to get their lives back! They want to return to activities they love without hip pain.
So, Does Surgery, in Fact, Resolve Hip Pain Problems?
Unfortunately, results from surgery were disappointing.
Twelve months after surgery, patients were asked whether their expectations were met. As you can see in the graph, there was a lot of disappointment:
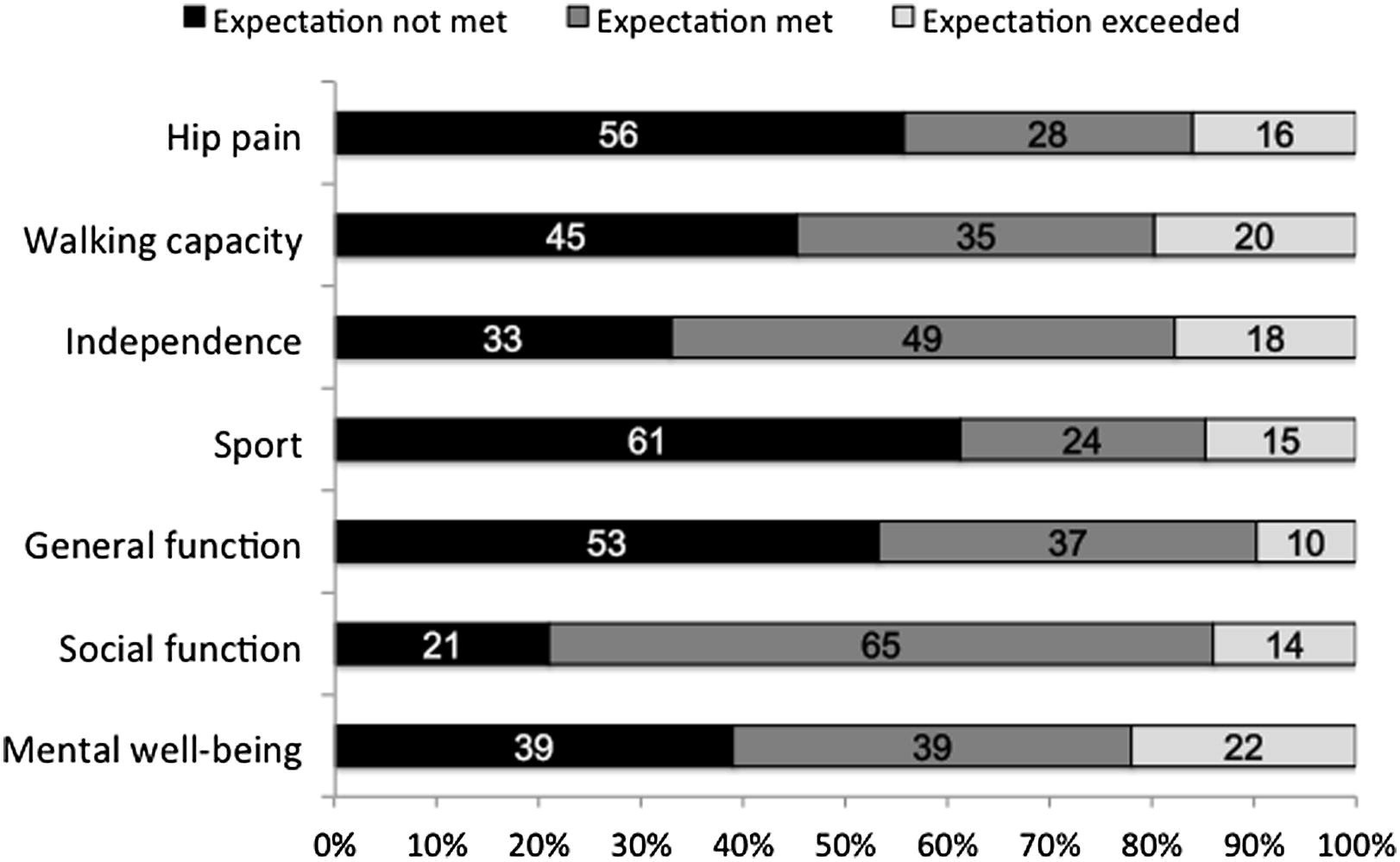
- 56 percent of patients did not have their expectations met for alleviation of hip pain
- 45 percent didn’t have their expectations for walking ability met
- 61 percent did not find their athletic abilities improved as much as they expected
- 53 percent were disappointed in terms of general function
The numbers are disconcerting. Surgery failed to deliver general function for daily life for more than half the patients! More than half the patients did not get the level of hip pain relief they expected.
Do Studies Show Patients Are Satisfied with Surgery for FAI?
What about a longer time horizon?
A study published in 2016, “Multicenter outcomes of arthroscopic surgery for femoroacetabular impingement in the community hospital setting,” looked at patient satisfaction after two years. It used the Nonarthritic Hip score (NAHS), a 100-point scale of perceived postoperative changes in pain, and daily and sports activities.
At the two-year mark, only 64 percent of patients were “satisfied”—better than a coin toss, but not by much. Yet the study concludes that "arthroscopic surgery for symptomatic femoroacetabular impingement in the community setting provides safe and successful outcomes."
If you read only the conclusion, you might think the study strongly supports use of surgery for FAI. But let's put the results into perspective.
- 36 percent of the patients were not satisfied—about one out of every three patients. Quite a lot.
Perhaps more compelling: Being "satisfied" may not mean the surgery actually improved a patient's quality of life. Understanding how the NAHS works explains why.
NAHS has 20 questions, each with five possible answers. A 4-point answer is the best and means you have great hip function. Conversely, 0 points correlates with the worst scenarios.
For example, one question is:
How much pain do you have walking on a flat surface?
4 = none
3 = mild
2 = moderate
1 = severe
0 = extreme
You answer all 20 questions in the NAHS, multiply your points by 1.25, and then get your final score out of 100, the best score.
In this study, the patients averaged 54.9 points before surgery, which correlates on average with around slightly over a 2 on every question (54.9 divided by 1.25 divided by 20 = 2.2). It’s reasonable to say they had moderate to mild issues with all the questions on the NAHS.
After the surgery, the total average score was 75.4. That’s about a 20-point increase, which seems significant. But in reality that jump correlates on average with slightly over a 3 (75.4 divided by 1.25 divided by 20).
In other words: The average patient’s problems went from “moderate” to “mild,” from 2.2 to 3.02. This is not improvement to the point of having no problems. It’s not even drastic improvement, yet it’s considered “successful.”
Dr. David Hanscom, MD, a spinal surgeon, shares a very interesting statistic in his book on the perils of spine surgery relevant to our discussion here: In one study, despite poor results from surgery, 16 percent of patients said they would choose to do the surgery again!
That means that even though surgery doesn’t improve someone’s situation, they can still be "satisfied"—because they tried the only option that medical professionals presented to them.
This is very likely influencing hip surgery satisfaction rates as well.
Randomized Controlled Trials Show Little Benefit to Hip Surgery for Femoroacetabular Impingement
If we look at the few randomized controlled trials comparing arthroscopic hip surgery to nonsurgical treatment, we see that surgery is not that effective.
The hip impingement study with the longest follow-up period (Mansell 2018) showed no significant difference in outcomes between patients who got surgery and those who didn't. Patients in both groups reported no major improvement in their hip pain and function after 2 years.
For a detailed look at three randomized controlled trials on hip impingement, watch this video.
However, some studies have concluded that surgery produces slightly better results than physical therapy. But the slight superiority in outcome scores can be easily explained by biased scoring systems that favor surgery (like the Harris Hip Score and the iHot-33).
The outcome questionnaires are almost guaranteed to yield bigger score improvements for patients undergoing surgery because of specific psychometric questions that ask patients to rate their frustration levels, fears, and expectations about their hip pain getting worse. Because they've been told that the source of their pain has been surgically fixed, patients who get surgery will rate far higher than the physical therapy patients.
Physical therapy patients, on the other hand, will continue to rate lower on those questions because they have been told repeatedly that they still have bad bone shapes that require surgery to see any improvement. They will, of course, feel more frustrated, anxious, and fearful about their hip pain getting worse in the future.
In addition, researchers over-interpret minor score differences between surgical and non-surgical interventions as "clinically significant." Closer examination makes this highly questionable.
Watch this video to see a detailed breakdown of how skewed metrics make hip surgery look good.
Finally, the physical therapy protocols used in these randomized controlled trials are often terrible. The protocols start with the assumption that no improvement is possible. The exercises in the protocols have no logical progression to improve hip function. The patients are told to expect that no improvement is possible. And in some cases, patients are told they can switch to getting surgery in the middle of the study if they feel too frustrated with making no progress.
This video takes a deep dive into the Personalized Hip Therapy protocol which was used in several of the randomized controlled trials on hip impingement.
Does Hip Surgery Protect Your Hip Joint from Further Damage?
Doctors will often claim that hip surgery will prevent further damage to the hip cartilage.
In 2021, researchers published a paper claiming that surgery was a little better than physical therapy for treating Femoroacetabular Impingement. They compared two groups of patients with hip pain. One group got surgery; one got physical therapy.
What's unique about this study is that the researchers also looked at the state of hip cartilage before and after treatment (see Table 4).
After 12 months they found that 0 percent of the physical therapy patients had any significant worsening of their hip cartilage.
Meanwhile, 31 percent of the patients in the hip surgery group showed worsening in their hip cartilage.
Based on the data in this study, it's hard to argue that surgery for hip impingement will protect your hip cartilage. It's also hard to say that delaying surgery is risky, given this data and the science on FAI bone shapes, arthritis, and pain. If anything, it appears that avoiding surgery better preserves your hip cartilage.
FAI Surgery: The Bottom Line
As you can see from studies like these, surgery for FAI does not seem to be anywhere near as successful as reported in medical literature.
These studies suggest that dissatisfaction and unmet expectations are extremely likely with surgery for FAI. Again: In one study, over half the patients were disappointed by improvements in daily life and in sport. In another, more than a third were disappointed by the surgery overall.
Based on these outcomes, surgery for FAI should be considered only very cautiously and as a last resort.
In addition, we believe that these disappointing numbers are one more indication that the underlying theories for FAI may not be accurate. Not only is it clear that surgery underperforms expectations, but also multiple large-scale studies show no link between the FAI bone shapes, hip pain, arthritis, or restriction in hip mobility.
Non-surgical Hope for Hip Pain Sufferers
When I lived in San Diego, I met a mobility coach named Shane Dowd. Just like me, he had suffered with severe hip pain and limitations for years. We realized that if we combined our knowledge, we might be able to help others avoid surgery. We took everything we learned over that years-long struggle and condensed it into a DIY program to help other hip pain sufferers for less than the cost of two physical therapy sessions.
If you're looking for a solution to your hip problems that doesn't involve drugs, pills or surgery (and is money-back guaranteed to help you), check out the FAI Fix.
Are diagnostic tests and hip injections useful for solving hip pain allegedly caused by Femoroacetabular Impingement? Read about FAI Diagnostic Tests and Injections.
It's important to stay informed on the latest studies on the success rates of hip arthroscopy for FAI. As we come across more studies on surgical success rates for femoroacetabular impingement, we will update this list:
- Multi-centre randomised controlled trial comparing arthroscopic hip surgery to physiotherapist-led care for femoroacetabular impingement (FAI) syndrome on hip cartilage metabolism: the Australian FASHIoN trial (August 2021)
- Arthroscopic Surgery or Physical Therapy for Patients With Femoroacetabular Impingement Syndrome: A Randomized Controlled Trial With 2-Year Follow-up (May 2018)
- Hip arthroscopy versus best conservative care for the treatment of femoroacetabular impingement syndrome (UK FASHIoN): a multicentre randomised controlled trial (June 2018) and ANALYSIS HERE.
- Arthroscopic surgery or physical therapy for patients with femoroacetabular impingement syndrome: a randomized controlled trial with 2-year follow-up (February 2018)
- Systematic Review and Meta-analysis of Outcomes After Hip Arthroscopy in Femoroacetabular Impingement (January 2018)
- Multicenter outcomes of arthroscopic surgery for femoroacetabular impingement in the community hospital setting (July 2016)
- Fulfillment of patient-rated expectations predicts the outcome of surgery for femoroacetabular impingement (November 2012)
- Arthroscopic Femoroplasty in the Management of Cam-type Femoroacetabular Impingement (March 2009)
More Hip Impingement Resources
- Learn more about hip impingement bone shapes and the missing link between cam, pincer, and hip osteoarthritis in this article.
- Why does surgery for hip impingement appear better than physical therapy in research literature? Watch this video.
- What do 3 randomized controlled trials say about Hip Impingement surgery? Watch this video.
- For the shocking and inspiring story of an FAI surgery patient and his post-surgical recovery, watch this interview.


